Biceps Tendinitis
Biceps Tendinitis
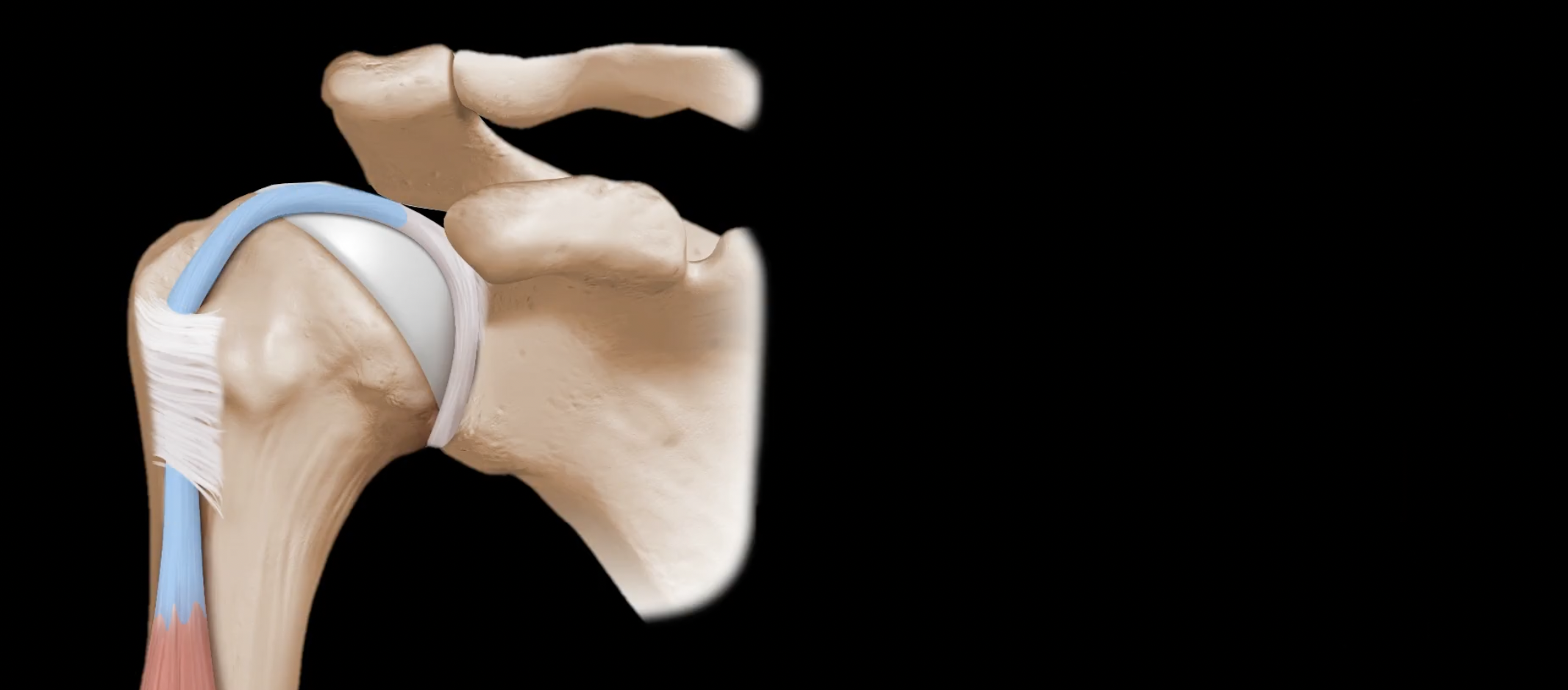
The biceps muscle originates from the shoulder at two separate locations. As its name suggests, the biceps has two distinct muscle components that arise from these two origins - a long head and a short head. The short head of the biceps muscle arises from a bone called the coracoid process, which lies outside of the shoulder joint. In contrast, the long head of the biceps tendon is one of the few tendons in the human body that actually travels inside a joint.
Due to this unique anatomy, the long head of the biceps tendon is vulnerable to injury and inflammation in a number of ways. Within the joint, it lies right under the supraspinatus tendon, which is the rotator cuff muscle on the top of the shoulder. Therefore, biceps tendon pathology is commonly associated with rotator cuff disease. If there is a full-thickness tear of the supraspinatus tendon, for example, the biceps tendon is then exposed to impingement from the acromion.
In addition, at the front of the shoulder, the long head biceps tendon runs inside of a tight tunnel called the bicipital tunnel. Therefore, any inflammatory process in the shoulder can lead to inflammation and swelling of the tendon, leading to entrapment within tunnel and more inflammation. In this area, the long head biceps tendon also lies adjacent to the subscapularis, another one of the rotator cuff tendons. The biceps actually relies on the subscapularis for stability within the biceps tendon groove. In cases where the subscapularis is torn, the long head biceps tendon will commonly dislocate out of its natural position.
Finally, the biceps tendon is attached to the top of the glenoid labrum, which is an area that is also vulnerable to injury with repetitive stresses of the biceps tendon being transferred to the labrum. Particularly in throwing and overhead athletes, the labrum in this area can become detached from the glenoid bone, in a condition called a SLAP (superior labrum anterior-posterior) tear.
Orthopedic Surgeon and Sports Medicine specialist, Dr. Jonathan Koscso, successfully diagnoses and treats patients in Sarasota, FL and the surrounding Gulf Coast region who are experiencing biceps tendinitis.
For a comprehensive overview of the relevant anatomy, biomechanics, and treatment considerations for biceps tendon pathology, the below video is quite helpful.
Symptoms of Biceps Tendinitis
Patients with biceps tendon disease typically experience pain at the front of the shoulder, which can radiate down into the biceps muscle. The tendon is also usually tender to palpation. There are several provocative physical exam maneuvers that reproduce pain with bicep tendon disease, which Dr. Koscso would test for during your consultation.
Non-Surgical Treatment of Biceps Tendinitis
We generally recommend beginning with non-surgical treatment for biceps tendon disease. Treatment may include activity modification (resting from activities that provoke the pain in the front of the shoulder), physical therapy, and oral anti-inflammatory medications (NSAIDs such as ibuprofen, naproxen, meloxicam, etc.). If symptoms continue to persist, then an ultrasound-guided injection of cortisone into the biceps tendon sheath may be considered as well.
Surgical Treatment of Biceps Tendinitis
If biceps tendon disease continues to be symptomatic despite non-operative treatment, then surgery may be considered. Given the close association between biceps tendon and rotator cuff pathology, these are often addressed at the same time if surgery is planned. Likewise, in certain athletes with biceps disease associated with a SLAP tear, a careful approach will be undertaken to adequately address both conditions at the time of surgery.
Surgical treatment for biceps tendon pathology in the shoulder can be thought of in terms of two primary techniques - biceps tenotomy or biceps tenodesis.
Biceps tenotomy involves releasing the tendon from its origin at the glenoid labrum, and simply letting it settle and heal in place. The advantage of the tenotomy is generally quicker and easier post-operative rehabilitation, with less restrictions. The main disadvantage, however, is that patients commonly develop what is called a “Popeye” deformity - since the biceps tendon is no longer anchored in the shoulder, the biceps muscle will contract against the unanchored tendon and form a bulge close to the elbow, like the Popeye character. This generally does not have any functional consequences, but it can be a significant cosmetic deformity, particularly in thin patients.
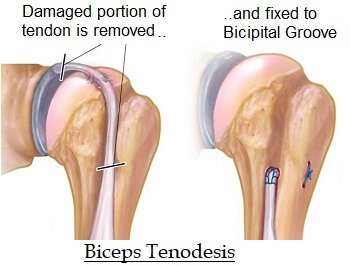
Biceps tenodesis, on the other hand, involves removing the portion of the tendon that is within the joint and reattaching it at a separate location into the humerus bone. This can be done arthroscopically or through a small incision at the front of the shoulder. Relative to tenotomy, biceps tenodesis maintains the mechanical function of the biceps, with a significantly lower incidence of Popeye deformity after surgery. The disadvantage of tenodesis is that it does require the tendon to heal to bone, which means that the repair must be protected after surgery through certain restrictions and guided physical therapy.
As always, each patient’s case is unique, and we hope this information is helpful for gaining an understanding of biceps tendon disease and potential treatment options. We would be happy to consult with you virtually or in-person, to review your situation in detail and answer all of your questions.
About the Author
Dr. Jonathan Koscso is an orthopedic surgeon and sports medicine specialist at Kennedy-White Orthopaedic Center in Sarasota, FL. Dr. Koscso treats a vast spectrum of sports conditions, including shoulder, elbow, knee, and ankle disorders. Dr. Koscso was educated at the University of South Florida and the USF Morsani College of Medicine, followed by orthopedic surgery residency at Washington University in St. Louis/Barnes-Jewish Hospital and sports medicine & shoulder surgery fellowship at the Hospital for Special Surgery in New York City, the consistent #1 orthopaedic hospital as ranked by U.S. News & World Report. He has been a team physician for the New York Mets, Iona College Athletics, and NYC’s PSAL.
Disclaimer: All materials presented on this website are the opinions of Dr. Jonathan Koscso and any guest writers, and should not be construed as medical advice. Each patient’s specific condition is different, and a comprehensive medical assessment requires a full medical history, physical exam, and review of diagnostic imaging. If you would like to seek the opinion of Dr. Jonathan Koscso for your specific case, we recommend contacting our office to make an appointment.